One homeless woman said she has been forgotten about, and left on medication that is not working for her.
Sandra said she has told the Health Service Executive (HSE) she is on the wrong medication, but nothing has changed.
She is one of the homeless people speaking out against the quality of the mental health services made available to them.
It is part of a wider report which interviewed 100 people experiencing homelessness.
Over half had engaged with a mental health service, but none were happy with the support they received.
Respondents were asked what their experience was like with the mental health service.
One person said: "I wanted to talk and get an answer. They gave me medication and I was left alone".
Another person said: "I went once. I was eight minutes with the doctor and he gave me tablets. I was really sick on them, so I sold them".
And another person remarked: "I am in addiction and all I get offered is more meds - I am suicidal and can't cope".
Newstalk's Kacey O'Riordan spoke to Sandra, who went into the care of the HSE when she was 13-years-old.
She is now 37 and still trying to make her way out of homelessness. She told The Hard Shoulder she feels she is not being listened to.
"There's been a time where they just gave me a medication where I was only after having my child, and I was that zonked that I couldn't even hold my child in the hospital because that medication was so bad.
"I went back and told them that I couldn't take that medication, and they left me on it - where I just stopped going and collecting it.
"So they just weren't bothered.
"That's the most annoying part of this: they don't bring you back to ask you 'How are you coping'.
"They always say to you, when they put you on the medication, that you might feel a bit worse in the way you're feeling of your depression and that.
"You might feel a bit more depressed and suicidal or whatever.
"But then they're not calling you back and asking you 'How are you feeling? Is this working for you?'
"They just leave you on that medication and just forget about you".
'It might not even be medication I need'
Sandra said she feels she is stuck in a cycle.
"I've cried... I've had four people in a room with me where I was like 'I need this help and yous aren't providing this help', and they'd give me another medication and forget about me again.
"So it's just a repeat of the same thing over and over again.
"I've been on anti-psychotic tablets where I'm not psychotic at all, I'm just depressed.
"I've looked up my medications, there was a medication where I was being real zonked... and it was an anti-psychotic, it wasn't even for what I needed it for".
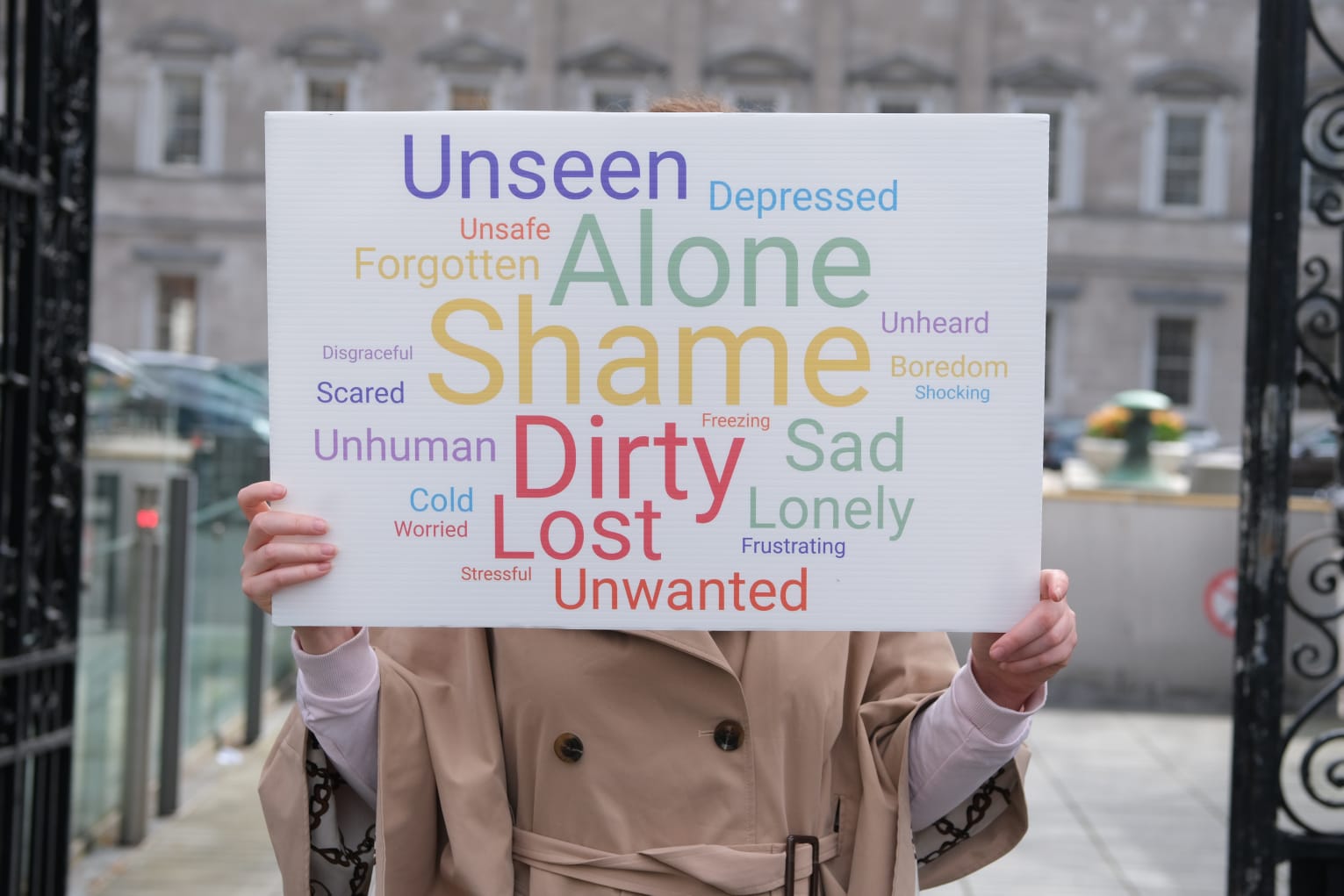 The launch of the 'Empowerment to Rights' report, a collaboration between the ICHH and BABS. Picture by: @ICHHDUBLIN on Twitter
The launch of the 'Empowerment to Rights' report, a collaboration between the ICHH and BABS. Picture by: @ICHHDUBLIN on TwitterSandra said she went back to raise the issue four months ago, and she has yet to have a review of her medication.
She thinks counselling, rather than medication, would improve her mental health.
"Sit and talk and listen to the problems, and then see what medication [could work] - and it might not even be medication I need, it's probably just counselling or somebody to listen to what's going on with me.
"It's probably not even medication, and that's why it's not working for me."
Sandra added she would "definitely" prefer counselling sessions over medication "if it worked".
"Who would want to be on a medication if it's not the right thing for you?"
'We are funding somebody's addiction'
William Cummings is from the BABS Empowerment Project, a listening and advocacy service for homeless people in Dublin city.
He ended up addicted to painkillers for seven years, at one stage he was taking 16 a day.
He said he was on the brink of homelessness when his family pulled together and arranged for him to get therapy.
He thinks the approach to mental health services for the homeless is all wrong.
"I would say to them, from my own personal experience and from people coming into me, we are basically funding somebody's addiction.
"They funded my addiction - I was addicted to painkillers - I could go and get them off my doctor, I could go and get them on every prescription I wanted.
"I was lapping it up, nobody asked why.
"We are funding addiction, and it's the reason why BABS, ICHH - all the homeless services - all talk about the fact that homelessness and mental health has become an industry.
"It's become an industry, and we are making clients for that industry."
"I would ask the HSE to look at this report and to come back and tell us why: why are we giving people medication that isn't working? And give an honest answer as to the reasons why".
HSE response
In response, the HSE said it has Specialist Homeless Mental Health Teams across Dublin, Cork and another is being developed in Kerry.
There is also a mental health team based in Galway, and community mental health nurses based in Limerick.
It said: "Counselling is available to homeless persons through a national service, Counselling in Primary Care (CIPC).
"Counselling is also available through the HSE Addiction Services and by HSE funded NGOs.
"In 2018 the National Office of Suicide Prevention (NOSP) provided additional funding for a homeless specific out of hours counselling service.
"Primary care open access services are also delivered through HSE funded NGOs and primary care inreach teams that provide GP and nursing clinics onsite in emergency accommodations, which have been expanded with additional mental health nursing clinics".
It added that the HSE Social Inclusion funds Safety Net - a primary care in reach team that provide services to the homeless population in emergency accommodation.
It said: "The team includes GPs, a mental health nurse and general nursing staff.
"Merchant's Quay Ireland also receive funding from the HSE to provide services to the homeless. They provide an open access drop in service providing GP clinics and mental health support.
"Given rapid changes to service delivery during the COVID-19 pandemic, the HSE National Social Inclusion Office (NSIO) along with the HSE Homeless Advisory Governance Group (HAGG) coordinated a National COVID-19 Homeless Service User Experience survey between March and June 2020.
"Over 400 service users completed the survey and the results give a voice to service users and will support evidence-based care and improve the quality and safety of care to the service user.
"Findings will not only help to inform service planning throughout the on-going pandemic, but will also provide guidance in relation to ongoing HSE service planning and quality service improvement in order to achieve an integrated and person-centred health service system for those experiencing homelessness across Ireland."









